

Therefore, these studies represent more serious fractures and risk of complications. Buckle fractures were specifically excluded from these two studies. These two studies look at greenstick fractures and/or transverse fractures of the distal radius that are minimally displaced. Now let us jump ahead to some more recent literature. The authors conclusions were ” Children treated with removable splinting have a better physical functioning and less difficulty with activities than those treated with a cast.” They could not blind researchers to parts of the ASKp tool, there was high loss to follow-up and no intention to treat analysis. There were some significant limitations to this study.
This study had n=87 with average age 9 years old. casting for wrist buckle fractures in children. They published a RCT of removable splinting vs.

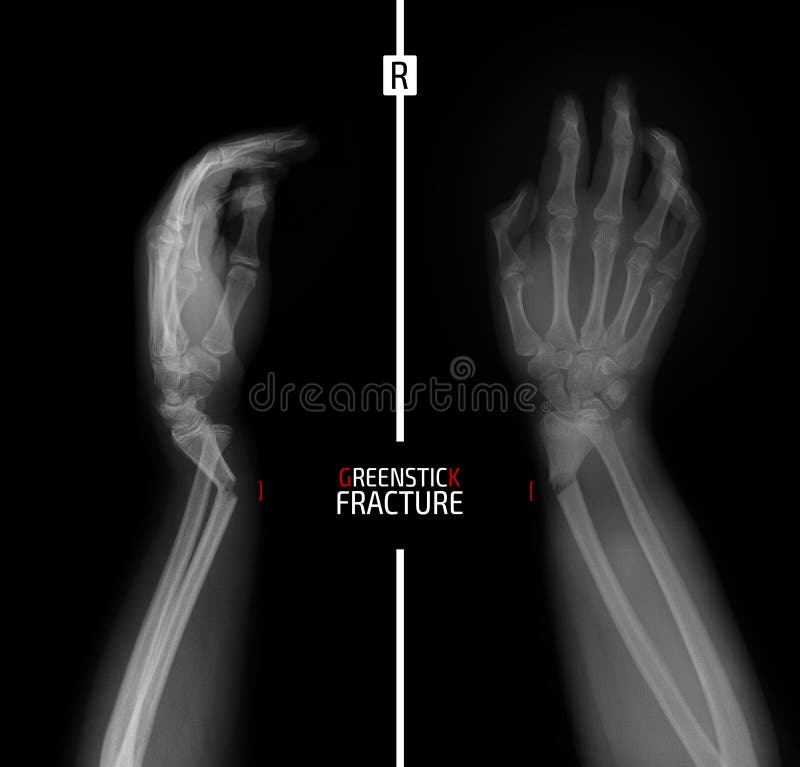
#Greenstick fracture distal radius trial#
Plint et al rose to the challenge of a prospective trial in 2006. A prospective study comparing ED splinting and casting for pediatric wrist buckle fractures is needed”. Splinting in the ED with primary care follow-up appears to be a reasonable management strategy for these fractures. ED casting may pose more risk than benefit for these children. With these limitations the authors concluded “Orthopedic follow-up visits and radiographic follow-up may have minimal utility in the treatment of pediatric wrist buckle fractures. In addition, 11% of patient were lost to follow-up. There are limitations to a retrospective study being conducted at a single site. 12% in casted group had subsequent ED visit for cast problems.Orthopedic visits (time for parents and child).Plint et al (2004) mentioned earlier published a retrospective chart review of 309 children with buckle fractures of the distal radius or ulna. The academic centre was AWARE of the evidence but did they ACCEPT, AGREE, able to ACT upon or ADHERE to the evidence? This is one of the key leaks in the Pathman pipeway.
#Greenstick fracture distal radius full#
The father of the patient told me the doctor at the peds emerg said splinting would be OK but they were going to put a full cast on anyways. This case was an excellent opportunity to address this knowledge translation problem. Why discuss such old data from nine years ago? As SGEM listeners know it takes an average of ten years for high quality, clinically relevant inforamtion to reach the patients bedside. I want to mention these before the critical review of two more recent articles on the subject. Looking back through the literature without commenting on every single article on the subject here are some highlights. Andrew Worster from McMaster always says…the EBM answer is always “it all depends”. splint for buckle fracture and appropriate follow-up?Īs with most evidence based medicine (EBM) it can be a little messy. Europe (favour splinting) ( Plint et al 2006). There is even an apparent devide between North America (favour casting) ( Plint et al 2004) vs. A survey done over a decade ago in Canada demonstrated this variablity ( Plint et al 2003). There seems to be a variety of approaches to the treatment of buckle fractures(cast vs.


 0 kommentar(er)
0 kommentar(er)
